- START-UP
- Special Theme _ BIOMEDICAL
본문영역
Development of the
First and Best-of-its-class
Spinal Cord Injury Drug
SuPine Therapeutics Co., Ltd.
Every year, around the world, up to 500 000 people suffer a spinal cord injury (SCI), most often caused by car accidents, falls, violence, or sports. Yet, there is no proven treatment. A company, affiliated with UNIST has taken up the challenge and is producing meaningful results at the moment. That is SuPine Therapeutics Co., Ltd., a bio venture company led by Kim Jeong-beom, a professor of Biomedical Engineering at UNIST.
First and Best-of-its-class
Spinal Cord Injury Drug
SuPine Therapeutics Co., Ltd.
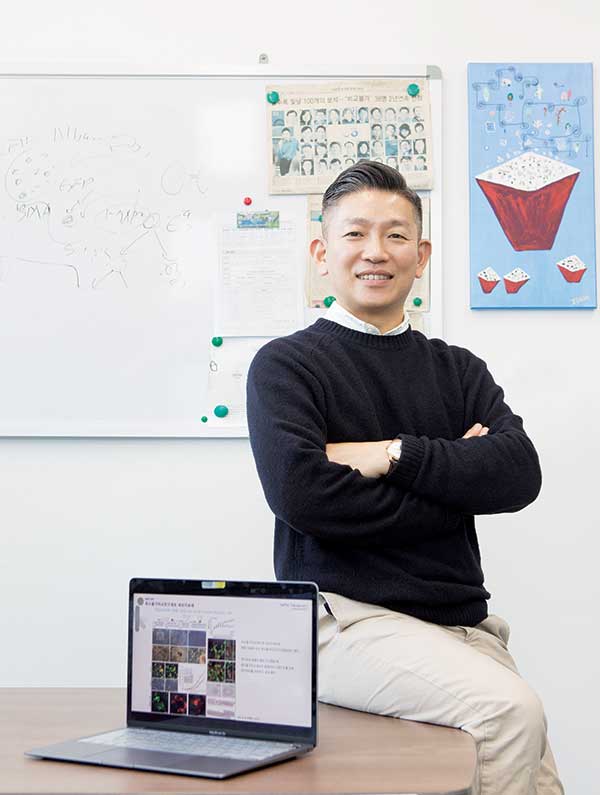 Kim Jeong-beom,
Kim Jeong-beom,a professor at UNIST’s Biomedical Engineering Department

In 2017, SuPine Therapeutics Co., Ltd. announced its foundation under the faculty-associated start-up program. Could you please introduce the company briefly?
A. __ SuPine Therapeutics Co., Ltd. is a venture company established with the aim of developing a first-in-class spinal cord injury drug. We have four major pipelines including our spinal cord injury drugs, veterinary drugs, patient-specific stem cell drugs, and the original technology of the organ tissue-assembloids platform. We are currently focusing on developing a biomaterial-based hydrogel treatment for spinal cord injuries.
Why did you focus on spinal cord injury drugs?
A. __Under the start-up’s motto of “Respect for Life, Recovery of Life,” SuPine Therapeutics was established as a research-oriented venture company that develops innovative treatments to help patients with incurable diseases return to a better-quality life, based on bioethics. First of all, we exclude diseases for which there is already a cure or a treatment from our research subjects. This is because it is difficult for a small bio venture company either temporally or physically to produce great results in a short period time; and also because it goes against the company’s founding spirit of respecting the lives of patients who are suffering from incurable diseases due to the lack of a cure.
How was the drug developed?
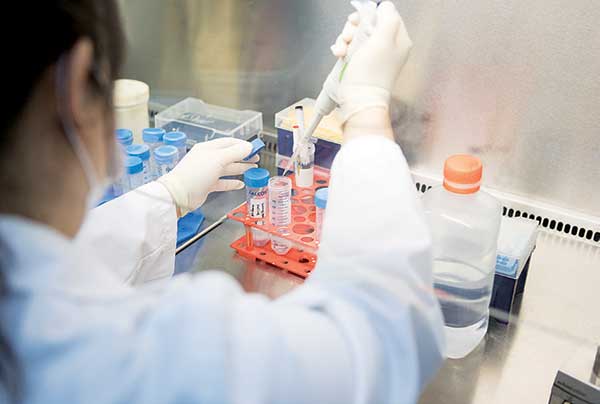
A. __ Personally, I started out in cancer cell research at the Cancer Center of the College of Medicine of Yeonsei University in 2000, where I conducted research aimed at producing a patient-specific stem cell that could be used to treat congenital and acquired diseases, while I was enrolled on a doctorate program at the International Max Planck Research School (IMPRS) in Germany. At that time, I developed a technology for reprogramming induced pluripotent stem cells (iPSC) from a patient’s skin cells, but this technology had carcinogenic potency. After entering UNIST in 2010, I developed “direct conversion”, a new patient-specific method of stem cell production that resolved the problems of the existing reprogramming method, and also succeeded in developing a safe method of stem cell production that is clinically applicable. Its result is our spinal cord injury drug. It started with the idea of developing an artificial spinal cord tissue that can replace damaged tissue during spinal cord injury treatment research. First, spinal cord cells were differentiated by direct cross-differentiation, making it possible to make all four types of cells that comprise the spinal cord from skin cells. When these cells are combined and reconstructed into a structure, it becomes a small spinal cord tissue. However, since the cells do not stick together, a biopolymer called hydrogel must be injected. We developed hydrogels tailored to spinal cord cells by selecting and formulating biopolymers suitable for the survival and growth of each spinal cord constituent cell.
As a result of transplanting the tissue made of the hydrogel and the directly cross-differentiated spinal cord cells into animals, it could be confirmed through numerous repeated experiments that the biopolymer hydrogel developed to aggregate the cells has a good therapeutic effect even without cells in the spinal cord injury animal model. The resulting hydrogel is a treatment for spinal cord injury.
With the biopolymer hydrogel stem cell treatment, on what principle is the treatment possible?
A. __ The best existing treatment for spinal cord injuries at hospitals was to remove the broken bones causing nerve compression, and the fix the spine. When the spinal cord is damaged, immune cells in the body gather to heal the damaged area, and the place where the immune cells heal the wound forms a sort of hole. If this hole is filled with nerve cells from the wound, the area hardens and thus the nerves cannot be reconnected. For example, the spinal cord is a derivative that transmits signals from the brain to each part of the body, but the damaged area acts like a non-conductor that blocks the electrical flow in the middle of the wire. As a result, before the nerve scar cells fill the wound, the hydrogel is inserted into the hole to prevent the nerve scar cells from filling the hole. As the hydrogel biodegrades, the hydrogel component induces the regeneration of nerve cells, providing a therapeutic effect by naturally connecting severed nerves.

What is its current stage of development?
A. __ The individual polymer that makes up the treatment developed by us is used in other treatments that have been approved by the FDA as safe, non-toxic substances. Although we have not yet conducted the Phase 1 clinical trial, we believe that, along with the FDA approval, we have already been given the green light. Based on such safety nature, we applied this treatment to laboratory mice with hind limbs paralyzed by spinal cord injuries, and verified the results in which their motor nerves and sensory abilities were revived. Now, we are conducting clinical tests with medium-sized animals. As a result of injecting the drug into a dog whose hind limbs were paralyzed by damaged discs, the dog recovered its motor nerves close to the normal state within just two weeks. Through the toxicity test we completed the in vivo non-toxic validation, and the freedom to operate (FTO) opinion on the drug’s components was analyzed, proving that there is no problem. At present, we are planning a GMP production facility for mass production of the hydrogels required for the Phase 1 clinical trial.
I guess there must have been a lot of difficulties during the development process. What was the most difficult part for you?
A. __ As this kind of technology does not yet exist anywhere in the world, it can be said that the entire process of development has been very difficult. Because you have to make everything yourself, from hydrogel to the medical equipment used to inject the drug. The fact that there is no cure or treatment so far means that most of the many attempts and developments have failed. There were many difficulties in that an enormous physical investment was required based on an uncertain hope. However, as the saying goes, “Where there’s a will, there’s a way,” and it all worked out unexpectedly well. In general, the therapeutic effect of a spinal cord injury drug must be verified in small animals with spinal cord injuries first, and then in medium-sized animals (usually pigs or dogs). Then, while we were trying to attract investment for it, the opportunity came to us and we were able to verify the therapeutic effect of our drug not with an animal model but with a real dog that had suffered a spinal cord injury and stayed for treatment at a veterinary hospital. Thus, we obtained the approval of the Institutional Animal Care and Use Committee (IACUC) to use our drug to treat a real dog patient. After the treatment, we received feedback and data from the veterinary hospital that it was very effective, leaving us even more convinced of the possibility of our drug.
What is the driving force unique behind SuPine Therapeutics that enables it to run without giving up even when the going it tough?
A. __ All of the employees at SuPine Therapeutics are researchers who have shared joys and sorrows together with me over eight years. In particular, I can confidently say that our company’s competitiveness at home and abroad is attributable to our two research team managers, who started an integrated master’s and doctoral course at UNIST, and developed technologies for producing a cell cure and a spinal cord injury cure and verified their therapeutic effects. Based on such lab technologies, they participated in their commercialization, and then joined SuPine Therapeutics after graduating from the doctoral program. Together with such professional talents, our company aims to develop patient-specific cell cures or tissue cures as new solutions for diseases that are currently either incurable or have the only one solution, such as an organ transplant, in order to develop scientific technologies that contribute to human life, which serves as our driving force.
Lastly, please tell us about the direction your company aims to follow.
A. __ The phrases that I learnt during litereature classes and still memorize is one of the reasons why King Sejong created the Hunminjeongeum, i.e. “It is my wish that all the people can easily learn these letters (Hangeul) and that [they] will be convenient for daily use.” When I think of it now, it seems that from that moment until today, I’ve always wanted to develop a technology that would change the world. The goal of SuPine Therapeutics is to develop treatments that do not yet exist in the world, to respect the bioethics of patients who are suffering without a treatment, and to return them to normal family life. In addition, as a professor and the president of a company, I think that my duty is to believe in myself in a series of processes and to grow our business into a company that can support its researchers, who spend their youth in a small lab space, and help them to maintain and enjoy a better quality of life.